Credentialing & Contracting
Medenet provides an affordable alternative to handling credentialing and contracting in-house. We know the process, we have the technology and we can devote the time necessary to compile documents, complete enrollment forms, track the process and follow-up as needed.
Medenet physician credentialing experts will streamline this process by performing in-depth research and obtaining all pertinent documents. With Medenet at your side, you will experience a smooth and speedy credentialing process.
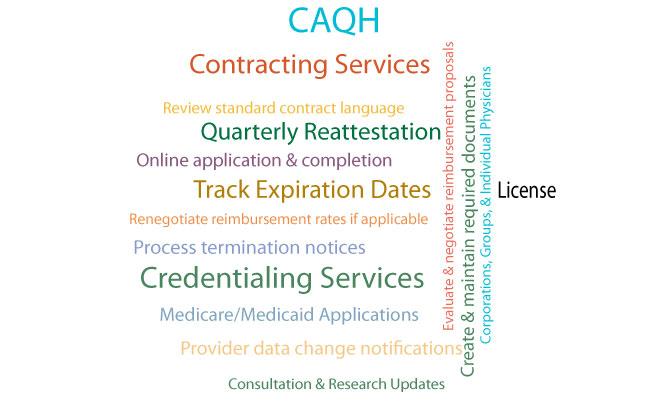
Credentialing Services
Medenet managed care and government payer contracting services include:
-
Set up and/or keep up-to-date CAQH profiles
- Monitor expirables with CAQH and payers including but not limited to licenses, DEA, malpractice insurance, hospital privileges
- Complete and submit unlimited enrollment applications and Hospital privileges applications
- Follow up on enrollment applications until processed
- Monitor CAQH profile
- Contract re-negotiation
- Individual Contracting (new contracts)
- Add new Providers to existing Group Contracts
- New Practice Contracting
Contract Negotiations
Medenet Practice Management staff has extensive experience with, and a deep understanding of, the managed care system. We will use our expertise and established industry relationships to help you negotiate contracts that are in line with the quality services you provide.